Four years ago, on March 11th, 2020, the World Health Organization declared COVID-19 a worldwide pandemic. With each respiratory season since then, the familiar specter of COVID-19 has persisted, but it is no longer the unprecedented emergency that dominates headlines. Instead, COVID has become part of the broader narrative of the respiratory virus season, sharing the stage with influenza and RSV.
The Respiratory Virus Season in 2023 – 2024
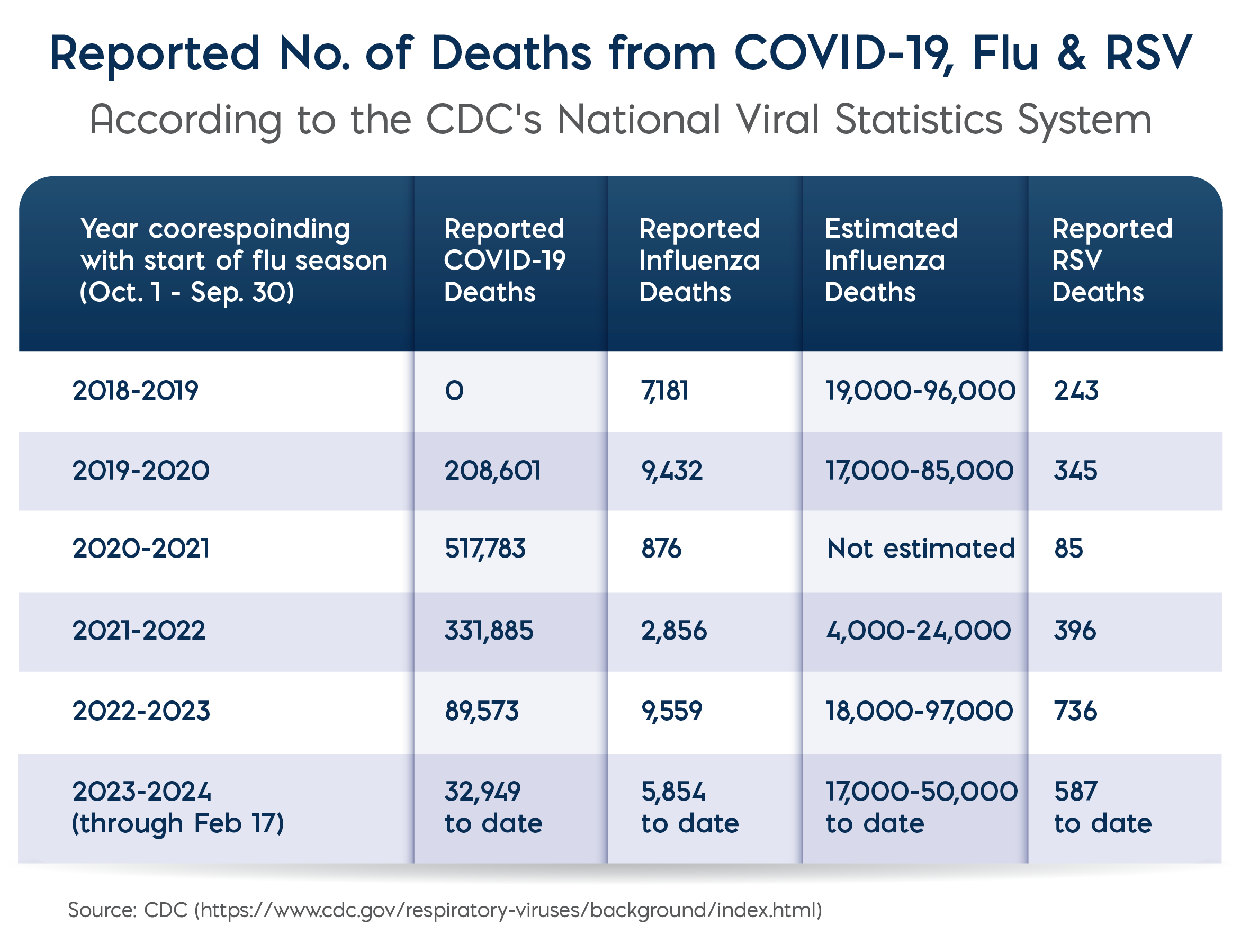
So far, this year’s respiratory season in the U.S. appears to be in decline, with most indicators trending down after a late surge in December. Compared to the 2022-2023 season, flu and RSV infections started later in the season this year, and while COVID levels are still higher than they were last season, other COVID metrics such as emergency room visits, hospitalization rates and deaths, are lower now than previous seasons. Overall, the most commonly reported influenza viruses this year have been type A(H1N1) and type B viruses.
Flu-related Pediatric Deaths
In early March, the CDC reported a further ten flu-related pediatric deaths, bringing the total for the season to 103. Over the past ten years, the number of pediatric flu deaths has ranged from 1 (2020-2021) to 199 (2019-2020) in a single season. This year, about half of the reported deaths (55) were associated with influenza A virus infection, and of the 31 influenza A specimens that were subtyped, 26 were influenza A(H1N1) and 5 were influenza A(H3N2) virus. Influenza B viruses were associated with 47 pediatric deaths this season. One death was associated with an influenza A(H1N1) virus and influenza B virus coinfection. Nearly 90% of the children who died were not vaccinated against flu .
In addition, for this respiratory season, China reported an increase in the incidence of mycoplasma pneumonia, predominantly affecting children. Although the circulating strain was mild, children were presenting with severe infections causing overcrowding in hospitals. The reasons attributed to this surge in M. pneumonia were (1) co-infections with other respiratory infections, (2) an immunity gap due to a lack of previous exposure during the COVID lockdown, and (3) resistance to macrolide antibiotics which are used to treat children infected with M. pneumonia. According to a study published in JAMA Network Open in 2022, nearly 80% of cases of M. pneumonia infections in China are resistant macrolide antibiotics, in contrast to less than 10% in Europe, America and Southeast Asia.
Extinction of the Yamagata Lineage of Influenza B Viruses
Up until recently, most flu infections were caused by variants from two influenza A strains—H1N1 and H3N2—as well as from two influenza B strains—the Victoria and Yamagata lineages. However, since March 2020, the Yamagata lineage of influenza B viruses has not been isolated and it is now believed to be extinct. All of the precautions that helped people avoid COVID such as masks, staying at home and better ventilation, appear to have impacted the Yamagata viruses, which were already in decline before the pandemic.
As a result of this change, in September 2023 the World Health Organization said that “inclusion of the Yamagata-lineage antigens in influenza vaccines is no longer warranted.” Accordingly, the U.S. FDA is recommending a three-strain flu vaccine for the 2024-2025 season as opposed to the quadrivalent vaccine that has been recommended for the past 10 years.
Major Shift in Respiratory Diagnostic Testing
As the flu season comes to a potential end in the northern hemisphere, the southern hemisphere is bracing itself for the start of its new season. Since November, monthly influenza cases in Australia have reached more than triple pre-pandemic levels, and the jump is largely thought to be due to increased travel to the northern hemisphere. However, predictions for the 2024 season are not available yet.
Since the pandemic, one major shift in respiratory diagnostic testing has been the adaptation of home testing for the flu and COVID-19. A range of home lateral flow tests are now available that can distinguish between flu and COVID with a single swab. In addition, syndromic molecular diagnostic assays that can simultaneously detect multiple pathogens or drug resistance markers, are replacing traditional panel-based ordering of infectious disease tests. Overall, rapid diagnostic solutions that expedite the identification and treatment of respiratory infections are gaining traction, modernizing the way healthcare providers diagnose and manage these conditions, ultimately leading to more efficient and effective patient care.
Meridian offers both highly sensitive and specific reagent solutions for rapid immunoassays and molecular (qPCR and LAMP) techniques to meet your needs. To learn more, visit our resource page:
References:
Centers for Disease Control and Prevention. “More than 100 Flu-Related Deaths in Children Reported So Far This Season” Centers for Disease Control and Prevention Wesbite. March 8, 2024.
Goodman, B. “The Covid-19 pandemic killed off one strain of the flu, and that will change the next vaccines” CNN Health. March 5, 2024.
Kim, K., et al. Global Trends in the Proportion of Macrolide-Resistant Mycoplasma pneumoniae Infections: A Systematic Review and Meta-analysis. JAMA Netw Open. 2022;5(7):e2220949. doi:10.1001/jamanetworkopen.2022.20949