Growing children don’t have time to wait.
Early diagnosis helps to quickly address the effects of lead exposure. Learn more about how you can protect your patients from the dangers of lead.
Who is at Risk
Lead is especially dangerous to children under the age of 6.
Children are considered at risk if any of the following are true:
- Child lives or frequently visits a home built before 1978. [1 in 4 children live in a home built before 1978]
- Child’s parent or primary caregiver works with lead.
Examples include: battery recycling or manufacturing, lead smelting, lead mining, auto repair, shipbuilding, construction, plumbing, and glass manufacturers. - Child has a sibling or frequent playmate with elevated blood lead levels.
- Child is a recent immigrant, refugee, or foreign adoptee.
- Child has a household member who uses traditional, folk, or ethnic remedies or cosmetics or who routinely eats food imported informally (e.g., by a family member).
Lifelong consequences of lead exposure include:1,2

Six times
higher likelihood of having a reading disability.

Seven times
more likely to drop out of high school.

Lower scores
on tests for math, reading, nonverbal reasoning and short-term memory.

Decline in IQ
with every 1.0 μg/dL increase in blood lead.
Have you found the children at risk in your practice?

1 in 38 U.S. children has harmful blood lead levels. Federal law requires that all Medicaid eligible children be tested at 12 and 24 months and ages 36 to 72 months if they have not previously been tested.

No safe levels. Evidence continues to grow that blood lead levels as low as 3.5 ug/dL may impair cognition, with no minimum threshold yet identified.

Early diagnosis helps to quickly address the effects of lead exposure and provides an impetus for lead abatement in homes.
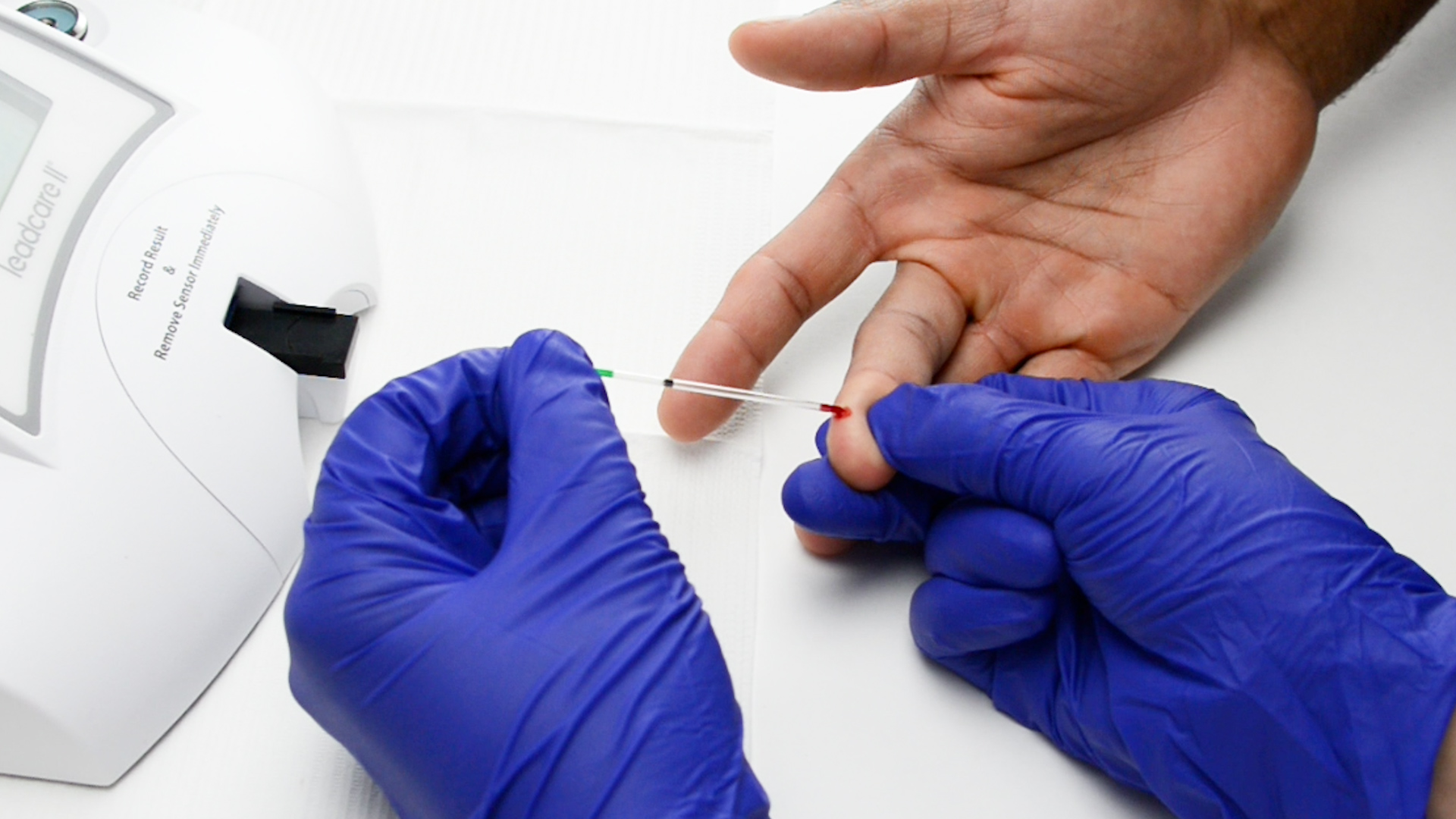
How is the testing performed?
A small amount of blood is taken from the finger, heel, or arm and tested for lead during a blood lead test.
A finger-prick (capillary) sample is usually the first step to determine if a child has lead in their blood. A capillary test is typically performed at the point of care, enabling the physician to act early should the test result come back elevated. A capillary test that generates an elevated lead level should be confirmed with a venous blood sample.
A venous blood draw takes blood from the child’s vein. It may take several days to receive results from the laboratory. Providers may order a venous blood draw to confirm the blood lead level seen in an initial capillary test.
All blood lead test results must be reported to the appropriate state or federal agency. The office/lab performing the test is responsible for reporting.

Point-of-care testing reaches those at risk, eliminating the need for follow-up.
Testing at the point of care enables you to detect harmful blood lead levels and take swift action in just one office visit.
Developed in collaboration with the CDC, LeadCare II is the only CLIA-waived system that allows you to test, educate, and intervene on the spot. Point-of-care testing makes it easy to comply with federal and state mandates. A LeadCare II test is also reimbursable, improving economics for your practice.
Lead results in 3 minutes.2 drops of blood. 1 visit. Zero loose ends.
What’s a Blood Lead Reference Value?
No level of lead in the blood is safe. In October 2021, the Centers for Disease Control and Prevention (CDC) updated the blood lead reference value from 5 ug/dL to 3.5 ug/dL.
CDC’s blood lead reference value of 3.5 µg/dL is a screening tool to identify children who have higher levels of lead in their blood compared with most children. The reference value is not health-based and is not a regulatory standard.
States independently determine action thresholds based on state laws, regulations, and resource availability. Learn more about CDC’s Blood Lead Reference Value.
CDC encourages healthcare providers and public health professionals to follow the recommended follow-up actions based on confirmed blood lead levels.
Learn about your lead testing requirements
The CDC provides resources to state and local health departments to support childhood lead poisoning prevention activities and strengthen testing efforts.
Click on a state below to visit your state’s Childhood Lead Poisoning Prevention Program webpage.
Frequently asked questions about lead exposure
What is lead?
Lead is a naturally occurring metal used in various products and materials. Exposure to lead, even in small amounts, can affect multiple body systems and be particularly harmful to young children.
How does lead exposure occur?
Lead exposure occurs when someone inhales lead-containing fumes or dust or swallows something that contains lead. Lead-based paint and lead-contaminated dust are the primary sources of exposure for U.S. children. Despite significant progress, lead poisoning remains a top childhood environmental health problem. (Source: Healthy Homes)
Why are children especially vulnerable?
Toddlers and young children explore with their hands and frequently put them in their mouths. As young children crawl on the floor and reach windows, railings, and walls, they may inhale dust from peeling and chipping lead-based paint or ingest paint chips.
Furthermore, children under six years of age are biologically more sensitive to lead due to rapid brain and organ development, when the body readily takes up lead—mistaking it for calcium. Therefore, children who are low in calcium or have iron-deficient anemia may have an ever-greater lead uptake.
Are adults affected by lead poisoning?
Adults can become lead poisoned, most frequently from the workplace and hobbies. Lead in adults can affect the central nervous and gastrointestinal systems and can cause chronic kidney disease as well as other health problems.
Is there any safe level of lead?
No level of lead in the blood can be defined as safe. An advisory panel of the CDC now recommends that children with blood levels as low as 3.5 μg/dL be identified as having elevated levels and be monitored. Even such low levels may harm a child’s cardiovascular, immunological, and endocrine health, with consequences for that individual and overall public health. While the effects of lead appear to be irreversible, eliminating lead exposure can reduce further damage.
What can I do to prevent lead poisoning?
The best way to prevent lead poisoning among young children is to remove the lead source. To prevent exposure, especially in homes built before 1978, the CDC recommends:
- Contact your local health department about testing paint and dust from your home.
- Ensure a child cannot access peeling paint or chewable surfaces painted with lead-based paint.
- Create barriers between children and lead sources until clean-up is complete.
- Regularly wet mop floors, damp sponge walls, and all horizontal surfaces and vacuum with a high-efficiency particulate air vacuum (HEPA vac). Cleaning is a temporary solution until the lead can be completely removed.
- Pregnant women and children should avoid pre-1978 homes if a renovation is underway.
- Regularly wash children’s hands, especially before eating.
- Regularly wash children’s toys.
- Prevent children from playing in bare soil, opting for sandboxes or planting grass. This is especially true of areas that are within one block of a major highway or busy street, as lead that was once in gasoline may have accumulated in the soil.
- Give your children foods that are high in calcium and iron, such as meat, beans, spinach, and low-fat dairy products. This can help reduce the amount of lead absorbed by the body.
Source: https://www.cdc.gov/nceh/features/leadpoisoning/index.html
Stay in the loop
Receive information regarding lead consumer alerts, policy updates, educational tools, and more!