Helicobacter Pylori (H. Pylori) Tests
Prevent the Preventable. Manage the Manageable.
H. pylori is 1 of 4 common infections that can lead to cancer- it is preventable with early detection.4
H. pylori is 1 of 4 common infections that can lead to cancer- it is preventable with early detection.4
Helicobacter pylori (H. pylori)
H. pylori is one of the most prevalent bacterial infections globally, characterized by typical gastrointestinal discomfort symptoms that can be treated. An H. pylori test is essential for accurate diagnosis and early intervention. When an H. pylori test is not conducted and the infection remains untreated, it may lead to the development of chronic gastritis, peptic ulcer disease, and even gastric cancer.5.
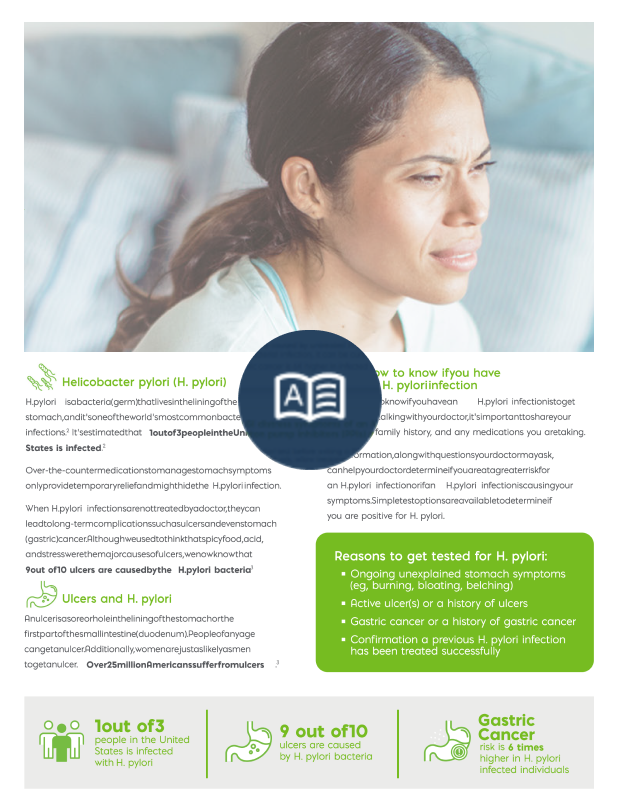
1 in 3 Americans are infected with H. pylori.1
9 in 10 ulcers are caused by untreated H. pylori infections.2
Gastric Cancer risk is 6 times higher in H. pylori-infected individuals.3
What is an H. pylori Test?
An H. pylori test is essential for detecting H. pylori, a bacteria linked to ulcers, gastritis, and stomach cancer. Early diagnosis with an H. pylori test helps prevent serious complications and ensures timely treatment. This H. pylori test is a simple, non-invasive procedure that provides accurate results for effective medical management. Regular H. pylori testing is recommended for individuals experiencing persistent digestive issues, as an H. pylori test can lead to early intervention and improved gut health.
Urea Breath Test Solution for H. pylori Detection
Noninvasive H. pylori test from a simple breath sample
Meridian Bioscience’s urea breath test platforms provide unparalleled flexibility and scalability for H. pylori test applications across diverse clinical settings. Discover customized H. pylori test solutions designed to meet the needs of high-volume reference laboratories or compact, near-patient clinical environments.
Only Meridian Provides a Complete H. pylori Active Infection Testing Solution
Meridian Bioscience provides the complete H. pylori testing solution that aligns with diagnostic standards set by the European Helicobacter and Microbiota Study Group (EHMSG) and Maastricht Consensus Reports9 and the American College of Gastroenterology (ACG)10, and other clinical guidelines. Our comprehensive testing menu includes non-invasive tests for active infection like the BreathID® urea breath test (UBT) and stool antigen tests, empowering healthcare professionals with accurate tools for diagnosing and managing H. pylori infections. Choose Meridian Bioscience for a dependable and efficient testing solution tailored to your needs.
Stool Antigen Test Solutions for H. pylori
Noninvasive test for the detection of H. pylori antigens in stool specimens
Meridian Bioscience's stool antigen testing solutions for H. pylori detection provide reliable, patient-friendly results without invasive procedures. As a leader in cutting-edge medical diagnostics, the Meridian stool antigen portfolio provides a precise and comprehensive method for identifying Helicobacter pylori infection, a critical factor in the management of gastritis and ulcers.
Learn More About H. pylori
H. pylori is one of the world’s most common bacterial infections and has common GI distress symptoms that are curable. If left untreated, an H. pylori infection can cause chronic gastritis, peptic ulcer disease and even gastric cancer.
Education and Outreach tools to learn more about H. pylori testing
As dedicated partners in enhancing patient care, we take pride in our diverse diagnostic portfolio and go further by offering educational content and tools, leveraging our expertise to boost testing utilization and support our partners comprehensively.
H. pylori, or Helicobacter pylori, is a type of bacteria that infects the stomach lining and can lead to various digestive issues, including gastritis and peptic ulcers.
Dyspepsia, commonly known as indigestion, refers to discomfort or pain in the upper abdomen, often accompanied by symptoms like bloating, belching, and nausea. It can be caused by various factors, including overeating, eating too quickly, consuming fatty or spicy foods, stress, or underlying digestive disorders. Dyspepsia can sometimes be a symptom of an H. pylori infection or other gastrointestinal conditions. If symptoms persist or worsen, it’s important to consult a healthcare provider for proper evaluation and management.
H. pylori is usually transmitted through contaminated food, water, or utensils. It can also spread through close contact with an infected person’s saliva or vomit.
Individuals experiencing persistent abdominal pain, bloating, or other symptoms suggestive of a stomach ulcer or gastritis should consider getting tested for H. pylori. Those with a family history of stomach cancer or peptic ulcers may also benefit from H. pylori testing.
Approximately 50% of the world is infected with H. pylori. When left untreated, patients with H. pylori are at risk for long-term consequences such as ulcers and gastric cancer. Gastric cancer accounts for about 1.5% of all new cancers diagnosed in the United States each year. Early detection of H. pylori is vital in establishing appropriate treatment.1,6,7
Guidelines from AGA and ACG recommend a test, treat, and retest approach to confirm the eradication of H. pylori. Active infection tests such as 13C-urea breath tests or stool antigens are recommended rather than serology (antibody). Serology tests cannot determine active H. pylori infection and are no better than a coin toss in predicting the presence of active infection.5,7,8
A healthcare provider will determine the most appropriate treatment for H. pylori. However, treatment may typically involve a combination of antibiotics and acid-suppressing medications to eradicate the bacteria and heal any resulting ulcers. The specific regimen may vary depending on the individual’s health and other factors determined by their healthcare provider.
The ACG/AGA guidelines emphasize the need to test for diagnosis, treatment, and retest to confirm eradication using a non-invasive active infection test for H. pylori infection. H. pylori eradication therapy fails in 1 out of 4 patients. Antibiotic resistance and poor compliance are considered the most common causes of H. pylori treatment failure. There are ways to detect active infection and confirm infection eradication of an H. pyloriinfection with our non-invasive active infection tests that deliver trusted results – for lifelong impact.5
Yes, H. pylori infections can recur, especially if the initial treatment was not successful or if the individual is re-exposed to the bacteria. Follow-up testing may be recommended to ensure the infection has been completely eradicated as determined by a healthcare provider.
While it’s not always possible to prevent H. pylori infection, practicing good hygiene, avoiding contaminated food and water, and adopting safe food handling practices can reduce the risk of transmission. Additionally, avoiding close contact with individuals who have active H. pylori infections may help lower the risk.
References:
- Fennerty, M. B. Helicobacter pylori: why it still matters in 2005. Cleveland Clinic Journal of Medicine, 2005; 72(Suppl_2), S1-7. https://doi.org/10.3949/ccjm.72.suppl_2.s1.
- Centers for Disease Control. MMWR (October 1997) Knowledge About Causes of Peptic Ulcer Disease—United States, March-April 1997.
https://www.cdc.gov/mmwr/preview/mmwrhtml/00049679.htm. Accessed June 9, 2022. - Helicobacter and Cancer Collaborative Group. Gastric cancer and Helicobacter pylori: a combined analysis of 12 case control studies nested within prospective cohorts. Gut. 2001 Sep;49(3):347-53. doi: 10.1136/gut.49.3.347. PMID: 11511555; PMCID: PMC1728434.
- The Lancet. Chronic Disease Management in Aging Populations. Available at https://www.thel ancet.com/journals/lancet/article/PIIS0140-6736(12)60790-9/fulltext. Accessed on June 9, 2022.
- Chey WD & Wong BCY. Practice Parameters Committee of the American College of Gastroenterology. American College of Gastroenterology guideline on the management of Helicobacter pylori infection. Am J Gastroenterol, 2007; 102(8):1808-1825
- American Cancer Society. Key Statistics for Stomach Cancer. Available at https://www.cancer.org/cancer/stomach-cancer/about/key-statistics.html Accessed June 9, 2022
- Chey, W. D., Leontiadis, G. I., Howden, C. W., & Moss, S. F. ACG Clinical Guideline: Treatment of Helicobacter pylori Infection. American Journal of Gastroenterology, 2018; 113(7), p1102. doi: 10.1038/s41395-018-0132-6
- Talley, N. J. American Gastroenterological Association Medical Position Statement: Evaluation of Dyspepsia. Gastroenterology, 2005; 129(5):1753–1755. https://doi.org/10.1053/j.gastro.2005.09.019